
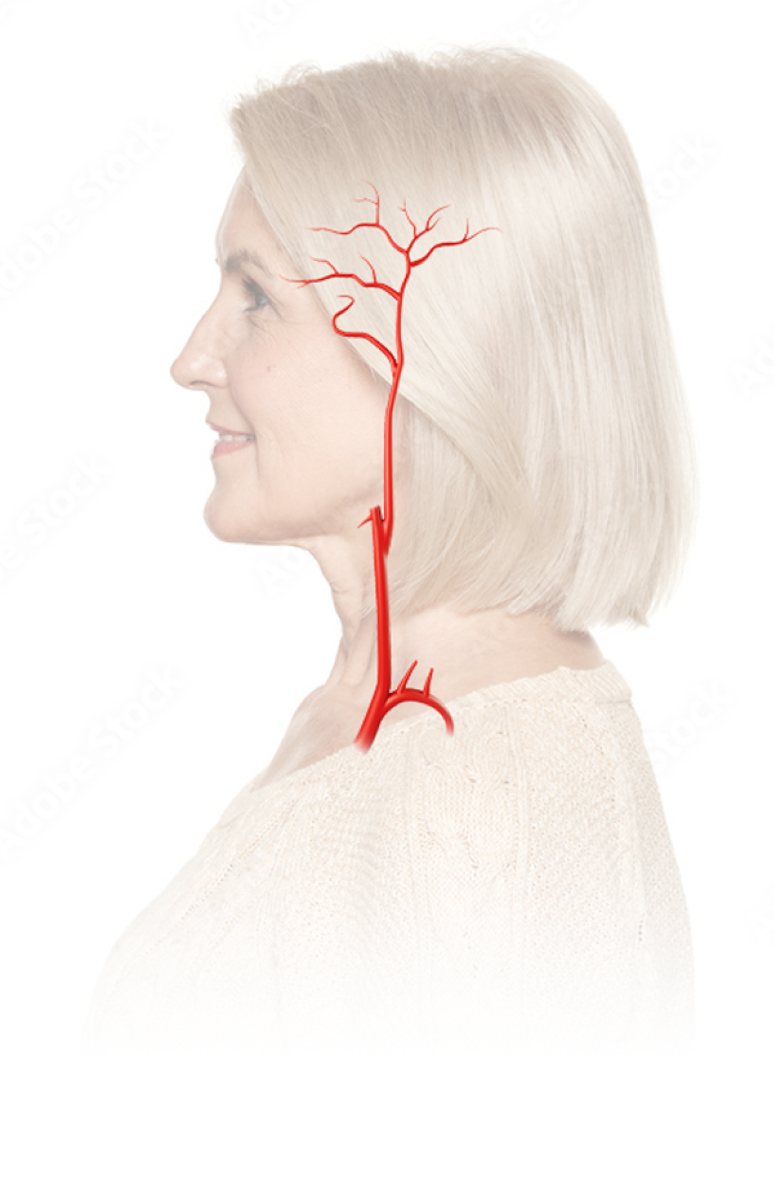
Symptoms That May Arise in Patients With GCA
Typical cranial
symptoms, 80%1
Scalp tenderness
Swelling and/or tenderness
of temporal arteries2Jaw claudation
Mandibular pain or pain
on chewingHeadache
Sudden or abrupt
unilateral headache3Ischaemic complications
Visual loss or impairment,
transient monocular/diplopia, or
optic neuropathy
Atypical noncranial
symptoms, 20%1
Extracranial symptoms (9%)
Limb claudication or subclavian steal syndrome, increased risk of long-term vascular complications (eg, aortic aneurysm, vascular stenosis, aortic dissection)
Systemic symptoms (9%)
Fever, anorexia, weight loss, and fatigue. GCA has been identified as a common source of fevers of unknown origin4
Isolated PMR with vasculitis (2%)
Asymptomatic vasculitis characterized by PMR symptoms
Pathways in the
Development of GCA
GCA, also called temporal arteritis, is a systemic inflammatory vasculitis of medium- and large-sized arteries.
Pathophysiology is thought to involve an inappropriate response to vascular endothelial injury with dysregulation of the innate and adaptive immune responses.
Though the cause is unknown, it is thought that an early insult to the endothelium activates the maturation of dendritic cells in the adventitia of normal arteries.
Activated dendritic cells release proinflammatory mediators that trigger the recruitment and differentiation of CD4+ Th cells into Th17 and Th1 cells.1,2
Th1 cells
Release IFNγ and TNFα, which are mediators of chronic inflammation that cause pathological vascular remodeling.
Th17 cells
Release IL-17, IL-22, and GM-CSF, which inhibit Treg cells, stimulating acute phase reactants and other immune cells.
Disease progression is characterized by expanding areas of inflammation within the lining of the arteries. This causes intimal thickening and inflammatory infiltrates leading to luminal narrowing, intimal proliferation, and disruption of the internal lamina.
- Immune-mediated disease resulting from a maladaptive response to endothelial injury
- Activated dendritic cells attract CD4+ Th cells and macrophages to the arterial wall
- Th17 cells stimulate monocyte differentiation into macrophages
- Th1 cells influence the formation of multinucleated giant cells, releasing IL-17, which inhibits Treg cells
- Macrophages, smooth muscle cells, and giant cells stimulate the release of PDGF, which is involved in the intimal hyperplasia, stenosis, and thrombosis of large vessels
Overview of pathological factors in GCA


Healthy temporal artery
Desktop Only:
This page is optimized for desktop viewing.
Please access it from a tablet or computer to enjoy the full experience.
